Conducting a clinical trial is a complex endeavor that involves numerous contributors, one of the most vital being the Institutional Review Board (IRB). Also known as an Independent Ethics Committee (IEC), an Ethical Review Board (ERB), or a Research Ethics Board (REB), the IRB plays a crucial role in safeguarding the rights and welfare of human research participants in the U.S.
What is an IRB?
Under Food and Drug Administration (FDA) regulations, an IRB is an independent group responsible for reviewing and monitoring biomedical and behavioral research involving human subjects. The primary purpose of an IRB is to ensure that the rights and welfare of research participants are protected. The IRB has the authority to approve, require modifications to, or disapprove research if it believes that participants’ rights or welfare are not adequately protected.
Historical Background
The concept of the IRB originated from several landmark efforts to incorporate ethical considerations into research. One of the earliest influences was the Nuremberg Code of 1945, developed in response to Nazi war crimes during World War II. U.S.-based events, such as the Tuskegee Syphilis Study, where Black men with syphilis were denied treatment, also highlighted the need for ethical oversight. This led to the enactment of the National Research Act in 1974, which formally established the IRB. The Belmont Report, following shortly thereafter, set forth the basic ethical principles underlying biomedical and behavioral research: Respect for Persons, Beneficence, and Justice. Today, the structure and function of IRBs are codified in 21 CFR Parts 16 and 56, enacted in 1981.
Composition and Membership
IRB members come from diverse backgrounds and may include lawyers, accountants, local church members, and other community members who express interest, apply for membership, and are accepted. Members can serve on private IRBs, or through academic institutions.
IRB Oversight in Clinical Trials
Both sponsors and independent researchers must comply with IRB oversight. Sponsors submit their protocol, information about the investigational product (IP), template consent documents, and any other materials intended for patients. Once approved, the IRB reviews the qualifications of the individuals conducting the research.
Each research site submits an application to the IRB to verify the investigator’s credentials, facilities, and staff. The submission should include the investigator’s curriculum vitae, medical license, study information, clinic details, staff involved in the research, expected participant numbers, and prior experience with similar trials. The IRB aims to confirm that each investigator is qualified to conduct the trial according to the approved protocol.
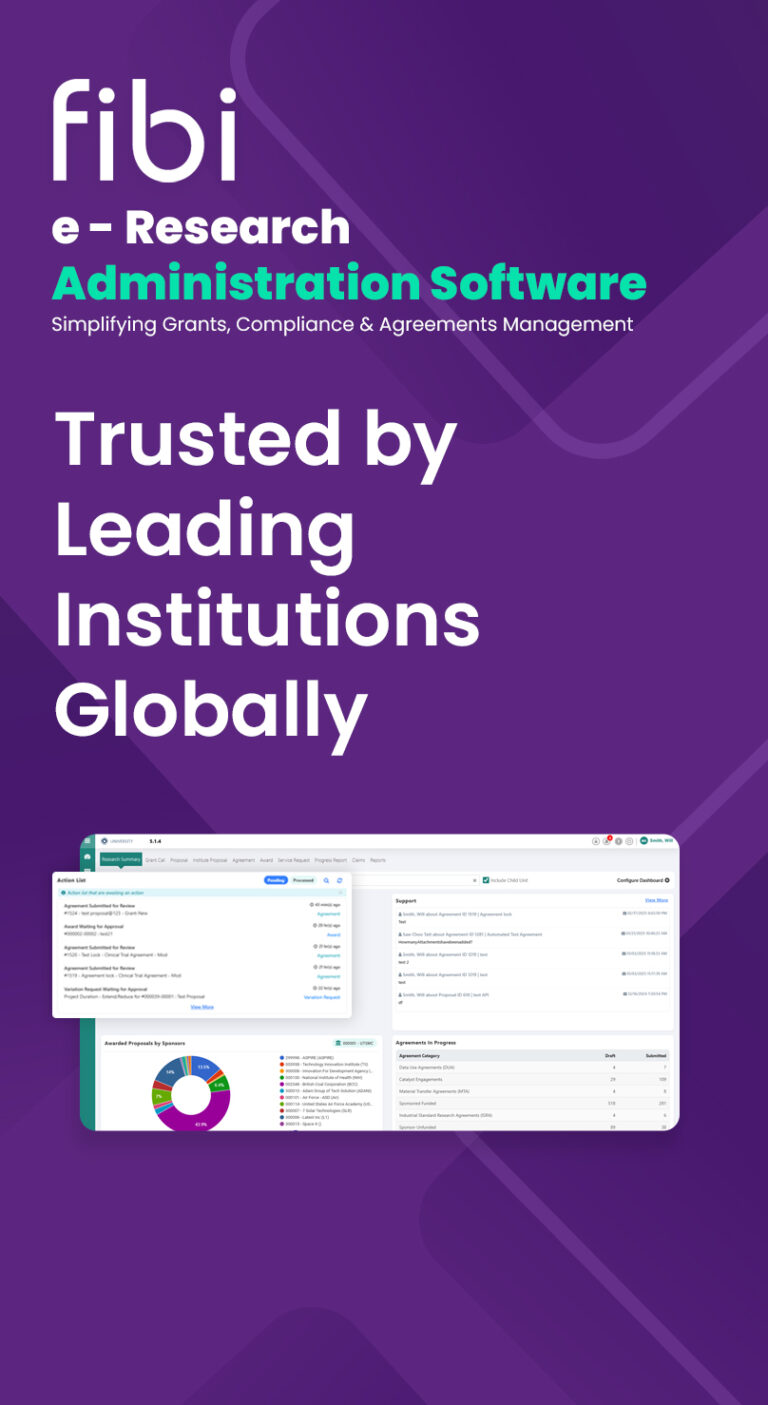
To smoothen the IRB process, organizations can benefit from using specialized electronic research administration software like Fibi. Fibi’s IRB module is designed to facilitate the entire IRB process, making it easier for research teams to manage submissions, track approvals, and ensure compliance with regulatory requirements. By utilizing Fibi, sponsors and researchers can enhance efficiency, reduce administrative burdens, and focus more on the scientific aspects of their trials.
The Role of the IRB in Research Continuation
While the IRB has the power to halt or terminate a research project, this is rare and not the primary objective. All the IRB members want to see projects move forward, new cures hit the market, and advancements in human health. If a protocol falls short, the IRB provides feedback and encourages the sponsor to update and resubmit the protocol. Sponsors can appeal the IRB’s evaluation or seek clarification if they disagree with its position.
Ongoing Monitoring and Communication
Once the protocol and investigators are approved, researchers begin enrolling and consenting participants. Periodic reports are sent to the IRB, detailing participant numbers and any issues arising. Significant interactions occur between investigators, sponsors, and the IRB when new risk information emerges. If new side effects are discovered, the IRB decides how to communicate this to participants and ensures they understand their right to withdraw from the trial based on the new information.
Long-term IRB Involvement
Even beyond the active participation phase, the IRB continues to monitor trial activities if there are interactions between researchers and participants. This includes long-term follow-up and data gathering. The ongoing oversight by the IRB provides participants with assurance that any new risk information will be promptly communicated, allowing them to make informed decisions about their continued participation.